For nearly twenty years, the science of aging has rapidly evolved from a niche field into a major global research discipline, driven by one central question: What is the biological key to living longer — and living healthier?
As laboratories worldwide intensify efforts to unravel the mechanisms behind longevity, a core scientific dispute continues to divide researchers: Should aging itself be officially recognized as a disease?
On one side of the debate, figures like Columbia University biologist Alan Cowen note that perspectives vary widely — from scientists who believe aging is a natural, untouchable biological process to others who envision pushing the boundaries of human life toward near-immortality.
Those advocating for aging to be classified as a disease argue that doing so could revolutionize medical research. Biologist Richard Farragher of the University of Brighton explains that diseases are traditionally defined as conditions that can be prevented, treated, or slowed, and argues that aging meets all three criteria.
Farragher notes that labeling hypertension as a disease in the past helped channel funding and focus toward therapies that significantly improved patient outcomes.
By applying the same logic to aging, he believes research could accelerate dramatically. He points to senescent cells — cells that stop dividing and accumulate with age — as a primary driver of chronic illnesses, from cardiovascular disease to cognitive decline.
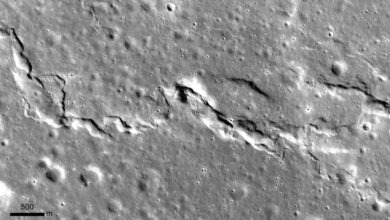
Removing these cells in animal models has produced remarkable gains in both health span and lifespan, suggesting that some components of aging may indeed be modifiable and reversible.
Supporters like Ming Gu, director of the USC Center on Aging, emphasize that formal recognition of aging as a disease would be a “game-changer,” opening the door to broader funding, regulatory clarity, and faster development of anti-aging therapeutics.
However, the opposing camp cautions that such a classification carries serious ethical and social risks. A proposal to add “aging” to the International Classification of Diseases (ICD) was withdrawn in 2022 after strong objections from physicians and researchers.
Critics fear unintended consequences. Kiran Rabhiro, a geriatric psychiatrist at the University of Ottawa, warns that labeling aging as a disease could fuel ageism, essentially categorizing all older adults as “sick.”
Mayo Clinic endocrinologist Sandeep Khosla adds that the classification may unintentionally shift patients away from proven interventions — such as exercise, nutrition, and blood pressure control — and toward an overreliance on pharmaceuticals.
As scientific discoveries continue to reshape our understanding of the aging body, the debate remains unresolved. What is clear, however, is that the quest to unlock a longer, healthier life is accelerating — and challenging medicine to rethink its most fundamental definitions.