The production of functional tissues using 3D bioprinting took another major step forward recently with scientists at the National Eye Institute (NEI) in the United States, using a patient’s stem cells and 3D bioprinting technology to produce healthy functioning eye tissue. The innovative technique is expected to further advance knowledge on the mechanisms of several diseases that lead to blinding.
The process of 3D bioprinting involves the use of bioinks, mixed with living cells, to produce functional tissues that are used to replace injured or diseased tissues. This technology, which has been witnessing rapid developments in recent years, is currently used in various research areas, such as tissue engineering and new drug development.
In 3D bioprinting, a natural or synthetic polymer with biocompatible components and favorable properties is selected to temporarily or permanently support living cells. This scaffolding facilitates the development of the cells during its maturation process.The bioinks can be stabilized during or immediately after 3D printing to generate the final shape, structure and architecture of the designed tissue construct.
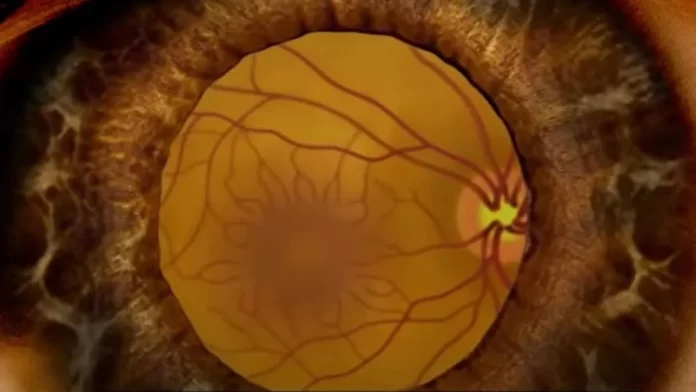
The research team from NEI printed a combination of cells that form the outer blood-retina barrier — eye tissue that supports the retina’s light-sensing photoreceptors. The technique provides a theoretically unlimited supply of patient-derived tissue to study age-related macular degeneration and other degenerative retinal diseases.
Age-related macular degeneration (AMD) is an eye disease that can blur your central vision, and occurs as either dry AMD or wet AMD. The disease happens when aging causes damage to the macula — the portion of the eye that controls sharp, straight-ahead vision. The macula is part of the retina , which is the light-sensitive tissue at the back of the eye.
Scientists have known that AMD starts in the outer blood-retina barrier. However, the mechanisms of initiation and progression of the disease to advanced dry and wet stages have remained obscure, mainly due to the lack of physiologically relevant human models.
The outer blood-retina barrier consists of the retinal pigment epithelium (RPE), separated by the Bruch’s membrane from the blood-vessel rich layer below. In AMD, lipoprotein deposits form outside the membrane, impeding its function. Over time, the RPE breaks down leading to photoreceptor degeneration and vision loss.
The research team combined three immature cell types — two of which are key components of capillaries, along with fibroblasts that give tissues their structure — into hydrogel polymers. The scientists then printed the gel on a biodegradable scaffold. Within days, the cells began to mature into a dense capillary network. Tissue analyses and genetic and functional testing showed that the printed tissue looked and behaved similarly to native outer blood-retina barrier.
The researchers said their collaborative efforts have resulted in very relevant retina tissue models of degenerative eye diseases, which could have many potential uses in translational applications, including therapeutics development. Besides using the printed blood-retina barrier models to study AMD, the scientists said they were now experimenting with adding additional cell types to the printing process, such as immune cells, to better recapitulate native tissue.