Hidden damage, real hope: Why Type 2 Diabetes can often be turned around
- Type 2 diabetes isn’t always forever: How weight loss and lifestyle changes can put the disease into remission
- From diagnosis to remission: The science behind reversing Type 2 Diabetes
Diabetes is a serious, life-threatening chronic disease that raises the risk of blindness, kidney failure, heart disease, nerve damage, stroke, and even amputations. But scientists are increasingly recognizing something encouraging: type 2 diabetes doesn’t always have to be permanent. With early action, many people can reverse the condition or push it into remission.
Today, one in 10 Americans and more than 830 million people worldwide live with diabetes. About 91 percent of these cases are type 2 diabetes, which typically develops in adulthood. Another major concern: one-third of Americans have prediabetes, and more than 80 percent don’t know it, according to National Geographic.
“Type 2 diabetes is like having termites in your home,” says Dr. Osama Hamdy of the Joslin Diabetes Center in Massachusetts. “It doesn’t show many symptoms at first, but it can cause significant internal damage over time. The good news is that if we catch it early, we can reverse it or induce remission.”
What goes wrong in the body
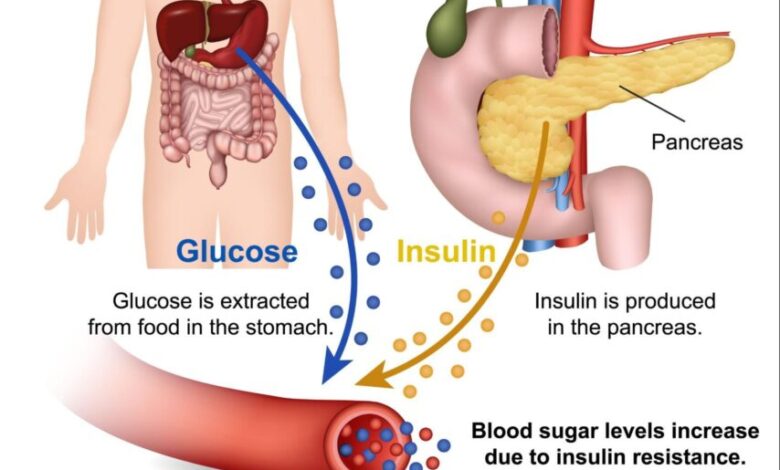
Type 2 diabetes develops when the body has trouble using insulin properly or cannot make enough of it.
Insulin is a hormone released by the pancreas after we eat. It helps move glucose (blood sugar) from the bloodstream into the body’s cells, where it’s used for energy. When this system fails, glucose builds up in the blood and becomes toxic.
“When someone has type 2 diabetes, this process isn’t working properly,” explains Dr. Sydney Blount of the University of Nebraska Medical Center.
Over time, excess glucose damages blood vessels and organs. This is why diabetes is a leading cause of dialysis, erectile dysfunction, dementia, blindness, heart attacks, strokes, and amputations, says Dr. Elizabeth Vaughan of The University of Texas Medical Branch. It is also linked to nerve damage, end-stage kidney disease, and several cancers.
Still, experts stress that these metabolic problems are largely reversible. “Modest weight reduction, reduced stress, a healthier diet, and more physical activity can restore normal function,” says Dr. Dariush Mozaffarian of Tufts University.
Why weight loss is key
Weight loss is the most effective path to diabetes remission. Insulin resistance is closely tied to visceral fat — the fat stored deep in the abdomen around organs like the liver and intestines.
“Visceral fat communicates with organs that regulate glucose, causing insulin resistance,” explains Dr. O. Kenrik Duru of UCLA.
Research shows that even a 7 percent reduction in body weight can improve insulin sensitivity by 57 percent, according to Hamdy. While Body Mass Index (BMI) is often used to estimate risk, experts note it’s not a perfect measure of overall health.
The power of exercise
Physical activity helps in two major ways: it supports weight loss and makes muscles better at absorbing glucose.
Exercise strengthens muscles and improves their ability to transport glucose from the bloodstream, boosting insulin sensitivity, Vaughan says. That’s why she often recommends a walk after meals.
The American Diabetes Association advises at least 2.5 hours of moderate exercise per week (or half that of vigorous activity), plus strength training twice weekly.
How diet and lifestyle changes help
Dietary changes can dramatically improve blood sugar levels by reducing spikes and slowing digestion.
Experts recommend:
- Cutting total calorie intake
- Reducing refined grains like white bread, rice, and pasta
- Eliminating added sugars
- Limiting high-glycemic foods such as crackers, noodles, certain cereals, corn, and potatoes
Instead, increase:
- Fiber, which slows glucose absorption and improves fullness
- Protein, which supports lean muscle mass
- Minimally processed foods and lean meats
- Water intake (around eight glasses daily) to help kidneys filter excess sugar
Sleep and stress also matter. “Lack of sleep and high stress both raise blood sugar,” says Vaughan. Aim for 7–9 hours of sleep and practice stress-reduction techniques.
A combined approach gives the best results, says Stanford endocrinologist Dr. Sun Kim.
How fast can remission happen?
At the Joslin Diabetes Center, a remission-focused program shows that 80 percent of participants achieve remission within two years, says Hamdy.
But improvements can happen much faster. People who lose significant weight may see remission-level glucose readings in days or weeks, similar to results after bariatric surgery. Even simple changes — like eliminating multiple sugary sodas per day — can quickly normalize blood sugar in newly diagnosed patients.
However, remission has a formal definition: blood sugar levels below the diabetes threshold for at least three months without medication, Kim explains.
And remission isn’t a permanent cure. The disease can return if weight is regained or unhealthy habits resume.
The bottom line
Type 2 diabetes is serious — but it is also largely preventable and often reversible. Early detection, weight loss, better nutrition, exercise, quality sleep, and stress control can restore healthy glucose levels and protect long-term health.
“Prevention is the best medicine,” says Blount.













