Averting AMR Protects Present, Secures the Future
The Times Kuwait Report
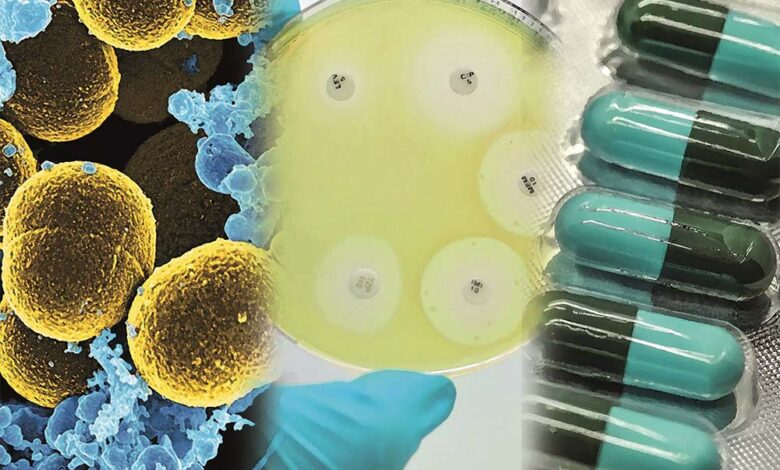
Antimicrobial resistance (AMR) is a major global health threat, with many bacterial, viral, fungal, or parasitic infections becoming increasingly difficult or impossible to treat. The growing inefficiency of medications against infection has been attributed largely to the use, overuse, and misuse of antimicrobial drugs in humans, animals, and agriculture over the last many decades.
Antimicrobial is an overarching term used to describe drugs that kill or inhibit the growth of pathogenic microorganisms such as bacteria, viruses, fungi, and parasites. Based on the microbes that they target, antimicrobials are categorized as antibiotics, which work against bacterial infections, antivirals that target viruses, and as antifungals or antiparasitics when used to treat fungi or parasitic infections respectively.
Since their widespread use in modern medicine, antimicrobials have become the preferred defense against various infectious diseases, saving hundreds of millions of lives every year and contributing to the increased lifespans worldwide. Developments in the field of antimicrobials have also transformed pharmacopeia, research, and treatment protocols, enabling successful outcomes to complex medical procedures such as cesarean births, organ transplants or chemotherapies.
However, repeated interaction with antimicrobials leads to microorganisms evolving and developing natural or acquired mechanisms to resist the drugs designed to kill or inhibit their growth, resulting in infections that are difficult or impossible to treat. Antimicrobial resistance (AMR) is the generic term used to describe the ability that pathogenic bacteria, viruses, fungi or parasites develop to withstand antimicrobial medications.
AMR undermines modern medicine by not only making common infections potentially lethal, but also increasing risks from routine or complex surgeries and therapies. Complications arising from drug resistant infections also lead to prolonged illnesses, longer hospitalization, higher mortality rates, and significant productivity losses, all of which come at high social and economic cost to individuals and communities.
According to data from the World Health Organization (WHO), AMR is directly responsible for 1.3 million deaths, and contributes to over 5 million AMR-related deaths every year. In addition, AMR is a threat to sustainable development and the economic future of nations, with the estimated global annual cost of AMR rising to US$3.4 trillion by 2030, driving an additional 28 million people to poverty by 2050.
In the Gulf Cooperation Council (GCC) states, AMR is a significant public health issue, driven by factors like high antimicrobial use, inappropriate prescribing and self-medication, a large international migrant workforce, pollution, and harsh environmental conditions. Significant deficits in comprehensive AMR surveillance, reporting, and appropriate responses are also a major concern in the region.
A study published in September 2022 on status of AMR in Kuwait, and on initiatives underway to address this major health concern, found a significant lack of accurate and updated data on AMR. While there have been several positive initiatives since then, there nevertheless appears to be a low understanding among the general public about the appropriate use of antimicrobials, and on its misuse.
Findings from an earlier study of 770 randomly selected Kuwaiti individuals to assess their knowledge, attitudes and practices regarding antibiotic use, was quite revealing. Although nearly three-quarter (73%) of the respondents had been prescribed an antibiotic over the previous 12 months, 36 percent failed to finish the prescribed course, mainly because they felt better. Antibiotics were also wrongly used without proper medical consultation by 27.5 percent of participants (187), to treat viral infections such as common cold or flu.
Equally concerning was the finding that there was confusion about whether antibiotics were effective against bacteria or viruses, and almost 47 percent had little knowledge about proper use of antibiotics and development of resistance. More work is clearly needed to generate greater public awareness on appropriate use of antimicrobial drugs. A multidisciplinary approach is essential to educate the public on proper AMR use; improve policies regarding rational prescription of antimicrobials; and increase regulatory control over AMR.
In its updated statement on AMR, which Kuwait submitted to the WHO in May 2024, the country outlined a National Action Plan (NAP) for reducing AMR. In the statement titled ‘Antimicrobial Resistance: Accelerating National and Global Response’, Kuwait noted that its plan exemplifies a robust ‘One Health’ framework, which engages stakeholders across multiple disciplines such as human and veterinary medicine, agriculture, finance, and environmental sectors.
The strategy includes implementing stewardship programs in major hospitals, enacting regulations to curtail inappropriate antibiotic prescriptions, fostering collaboration with international organizations, and escalating public awareness campaigns. Short-term goals aim to bolster AMR surveillance, extend its reach to the private sector, and initiate real-time data sharing by 2025.
Over the long-term, the strategy commits to align with WHO’s global action plan on AMR, aiming for a 50 percent reduction in AMR misuse by 2030. To its credit, unlike many other countries, Kuwait does not allow over-the-counter (OTC) dispensing of antibiotics, although admittedly this does occur to a certain extent. Nonetheless, there is a significant overuse of antibiotics in public health institutions and more so in private health facilities.
Health experts have opined that Kuwait needs a more standardized inclusive approach in developing local guidelines on AMR, using up-to-date surveillance data of isolates from community-acquired infections in the country. This would not only make AMR management guidelines more locally relevant for clinicians, it could pave the way for a higher level of appropriate antibiotic prescribing and improved adherence, potentially limiting AMR development and improving outcomes.
AMR is now a significant global health threat as drug-resistant microbes know no borders and can spread rapidly, exacerbated by factors like poverty, inequality, and natural or human-induced crises. AMR also heightens the mortality risk of patients with comorbidities such as diabetes, cardiovascular illnesses, obesity, lung conditions, neurodegenerative diseases, or other illnesses associated with microbial infections.
Additionally, unintentional use of antimicrobials to treat unrelated infections, for instance, using antibiotics to treat viral infections such as a flu, is not only futile, it could also potentially raise the risk of AMR. Antimicrobials also need to be taken in the dosage and for the duration prescribed by the physician, as stopping too early or using a smaller dosage, can allow some microbes to survive, evolve, and result in AMR development that subsequently could spread to the wider population.
Microbes that develop resistance to most available antimicrobials are sometimes referred to as ‘superbugs’. These resistant microbes can spread between people, animals, and plants across borders, and through the environment contaminate the food chain, resulting in the spread of resistant infections that could potentially lead to an infection pandemic.
Antibiotic Awareness Day is part of World Antimicrobial Awareness Week (WAAW), which is observed annually from 18–24 November. The week is dedicated to increasing global awareness of AMR and encouraging the responsible use of antimicrobials to prevent the rise of drug-resistant infections. The theme for WAAW 2025, ‘Act Now: Protect Our Present, Secure Our Future’, underscores the urgent need to take bold, united action to address AMR in the face of its negative impact on public health, food systems, environment, and economies.
According to WHO, to further the WAAW theme, we must prioritize long-term investment and strategic action in the human, animal and environmental health sectors. Strengthening surveillance, ensuring equitable access to quality medicines and diagnostics, fostering innovation and building resilient systems all require long-term commitment and resources.
AMR is not a future challenge that can be addressed later; it is a prevailing issue that needs to be tackled right now. Investment in AMR action today is also a smart move for a safer, healthier future. Together, we can keep antimicrobials effective and build a healthier, more sustainable world for the generations to come.












