While 2020 and 2021 may go down in the world’s collective memory as two harrowing years of infections, deaths and economic disruptions caused by the global pandemic unleashed by the SARS-CoV-2 coronavirus, 2022 will be remembered for the triumph of human ingenuity and solidarity, even if belated, in overcoming the virus.
The year 2022 also saw a wealth of other advances in medical research, including a new way of assessing potential dementia symptoms; an insulin-mimicking molecule that may in future help treat diabetes; innovative treatments using stem cell transplants; and, the use of certain psychedelic drugs for treating deep-rooted depression and anxiety, among others. Here we look at some of the medical breakthroughs in the year gone by.
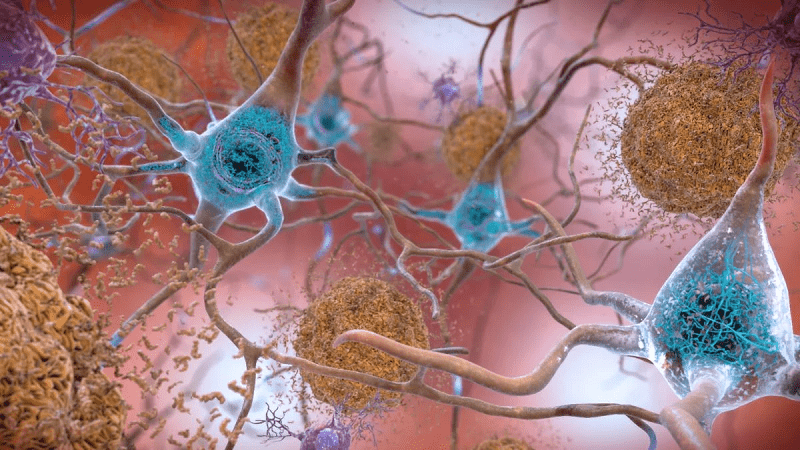
Breakthrough treatments in Alzheimer’s Disease: Over 55 million people around the world live with one form or another of dementia, including Alzheimer’s disease, which is the most prevalent form of dementia. While there are some treatments that target certain symptoms of dementia, such as memory loss and anxiety, there is currently no cure for Alzheimer’s disease and related neurodegenerative conditions. As such, the discovery of a new early warning system to identify the disease could be a remarkable development in treating Alzheimer’s.
Since the discovery in 2006 that an overaccumulation of beta-amyloid protein in the brain could trigger memory loss and thinking processes characteristic of Alzheimer’s, the ‘amyloid hypothesis’ has informed and guided research into treatments for the disease. The amyloid hypothesis maintains that beta-amyloid proteins form sticky plaques in the brain that disrupt communication between neurons, and thus affects memory and thinking.
However, in July 2022, researchers at Vanderbilt University in the United States claimed that some of the images in the seminal study conducted in 2006 had been manipulated, and could affect the credibility of the prevailing amyloid theory.
But proponents of the hypothesis maintained that the findings from the 2006 paper were very specific and, contrary to some reports, have not significantly affected the progress or direction of research into Alzheimer’s.
They point out that had the findings from the 2006 study not been reproduced in numerous Alzheimer’s cases since then, it would have been identified as controversial and lose credibility among the medical community. They add that the fact the hypothesis has been vindicated in findings worldwide, is the major reason why it has predominated and guided the direction of studies into treatments for the disease.
Supporters of the hypothesis also note that the recent development of the drug, lecanemab, which attacks the accumulation of beta-amyloid in the brain, and has shown clear promise in recent clinical trials as a potential early treatment for Alzhemer’s, attests to the importance of conducting further research, rather than abandoning the hypothesis.
Scientists admit that beta-amyloid plaques are not the be-all and end-all of dementia research, especially considering that beta-amyloid accumulates in the brains of healthy people as well. However, what makes this protein disruptive in some cases but not others is what remains unclear.
Researchers are also looking into alternative or additional pathologies in Alzheimer’s disease and other forms of dementia, including the role of tau, another protein implicated in dementia, which, some experts say, may be a better indicator of Alzheimer’s disease progression.
In other research into the debilitating disease, in September 2022, a separate study on animals suggested that brain inflammation caused by a dysfunction in the blood-brain barrier could be a likely cause of Alzheimer’s disease. And in November 2022, another study argued that disruptive swelling along axons, which form the link between neurons, may be the true cause of Alzheimer’s symptoms.
Stem-cell treatments: One emerging treatment for dementia is stem cell therapy. Stem cells have the potential to differentiate and ‘specialize’ into cells with different functions, thus providing healthy cells to replace those that have experienced ‘damage’.
Stem cell research made great strides in 2022, with scientists looking at the potential of stem cell treatment in many incurable or difficult-to-treat diseases.
In April 2022, a study showed how implanting induced pluripotent stem cells in rats with Parkinson’s disease-like motor symptoms helped reverse those symptoms by replacing damaged neurons. [Pluripotent cells that have the capacity to self-renew by dividing and developing into the three primary germ cell layers of the early embryo.]
Stem cell research has also reached other interesting levels in 2022. In August of last year, two different research teams reported having successfully created embryo models in the laboratory, using not sperm and egg cells, but stem cells to do so. The embryo models managed to develop rudimentary structures, including a beating heart, blood stem cell circulation, a head region with folds, and the beginnings of a gut tube. These developments were viable enough to encourage researchers to continue further studies along this line, in particular, since it steers clear of controversial experiments with potential ethical implications.
Other researchers managed to create brain organoids — models of brain tissue — from stem cells in the lab last year. These models could help scientists learn more about rare neurological conditions, or use models of brain tissue to better understand the way in which viruses, such as SARS-CoV-2, might attack and affect the brain, as well as to further dementia research.
Psychedelic Drugs: Another research avenue that has been gaining ground in 2022 is the use of psychedelics in the treatment of anxiety and depression. Data gathered from international studies show that hundreds of millions of people around the world live with anxiety or depression, which can severely affect their quality of life.
The standard treatments for these mental health conditions include psychotherapy and cognitive behavioral therapy (CBT), as well as medications known as anti-depressants such as serotonin, which help rebalance the levels of key chemicals in the brain. However, according to some estimates, up to 30 percent of adults living with major depressive disorder have treatment-resistant depression, which does not respond to standard lines of treatment. And around 50 percent of adults with generalized anxiety disorder do not respond to first-line treatments, such as antidepressants.
In a bid to find more effective ways of addressing the symptoms of hard-to-treat depression and anxiety, researchers have turned to a sometimes-controversial line of inquiry, namely psychedelics, particularly ketamine, LSD, and psilocybin, the psychoactive compound in ‘magic mushrooms’.
These drugs are, for the most part, illegal for personal use in most countries, but researchers are permitted to study their effects in humans under closely supervised, clinical trial conditions. Results of some of these studies have been intriguing.
Research studies note that since the human brain has a negativity bias — meaning it tends to hold onto negative memories and emotions — this may exacerbate the negative thinking that occurs in anxiety and depression. A study in October 2022 concluded that infusing ketamine can ease depression symptoms in as little as 4 hours by ‘updating’ negative beliefs that people with severe depression hold about themselves and the future.
Notably, patients started to show an optimism bias in belief updating 4 hours after the first, single infusion. At one week of treatment, the optimist bias in belief updating correlated to clinical antidepressant effect. And in November, another study found that a single, 25-milligram dose of a synthesized formulation of psilocybin also relieved the symptoms of treatment-resistant depression, although the exact way in which psilocybin acts on the brain remains unclear.
However, the researchers were quick to warn that while their studies indicate that psychedelics may be a potential treatment for anxiety, they also come with a series of caveats. Although ketamine infusion is available, it is not commonly used, and is reserved only for treatment-resistant depression, under strict medical supervision. Ketamine is also designated as a ‘controlled substance with inherent risks’.
Also, with regard to psilocybin, while it did help reduce depression symptoms in most of the participants, about a week after the treatment, the most commonly reported side effects were suicidal ideation and intentional self-injury.
The researchers warn that these treatments need to be done only by professionally trained, licensed, or certified practitioners who understand the power of these drugs to create a mind-altered state. In the course of studying psychedelic treatments, a few questions remain: What are the safest doses and delivery methods? Do the benefits outweigh the risks? And who would most benefit from these interventions?
We hope that in 2023, the world will make scientific advancements that take us closer to finding answers to these and other intriguing questions that could transform healthcare practices for the betterment of humanity everywhere.